1801006118 - LONG CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 50 year old male, resident of Miryalagudem , ice factory worker by occupation presented with the chief complaints of
Weakness in the right upper and lower limbs since 7 days
slurring of speech and deviation of mouth to the left since 7 days
HISTORY OF PRESENT ILLNESS:-
Patient was apparently asymptomatic 1 month back later developed giddiness and weakness of right upper and lower limbs followed by fall and diagnosed with hypertension during hospital admission.
Patient then developed sudden onset of weakness in the right upper and lower limb while going to washroom and he was swaying towards right side and unable to walk, associated with deviation of mouth towards left side and slurring of speech after few minutes and taken to the local hospital then referred to our hospital on next day morning.
Upper limb- Patient has difficulty in combing hair, difficulty in buttoning and unbuttoning
Lower limb- not able to stand due to swaying towards right side
No H/o difficulty in lifting the neck, rolling over the bed and no difficulty in breathing
No h/o tingling and numbness, patient is able to feel his clothes.
No H/o loss of consciousness, altered sensorium and headache, seizures and bowel and bladder disturbances
No complaints of memory or sleep disturbances and delusions
No H/o diplopia, blurred vision, drooping of eyelids, able to chew food and no difficulty in swallowing
Patient has no difficulty in closing eyes , lips, able to sense taste and able to move neck and tongue
No H/o fever, vomiting, headache , neck stiffness or any trauma to the head.
PAST HISTORY:-
Known case of hypertension since 1 month
Patient started using medication for hypertension for 20days and stopped for next 10days.
Not a known case of diabetes, asthma, tuberculosis, epilepsy, thyroid abnormalities,coronary artery disease.
PERSONAL HISTORY:-
Daily routine:
Wakes 4am in the morning and stays close to his workplace, breakfast around 8-9am, lunch around 2pm usually takes rice and curry in his meals and consumes chicken/mutton twice weekly. He comes home by 6pm evening and sleeps by 9pm
Diet - mixed
Appetite- normal
Bowel and bladder movements - regular
Adequate sleep
Patient consumes alcohol since last 20years and chewing tobacco since last 10years.
1 packet for 2days
DRUG HISTORY:-
Takes medication for hypertension- Atenolol and amlodipine for 20days after diagnosed with hypertension and stopped for next 10days.
FAMILY HISTORY:-
No similar complaints in family
GENERAL EXAMINATION:-
Patient was conscious, coherent, cooperative, well oriented to time, place and person.
Moderately built and well nourished.
Vitals-
BP : 140/90mm Hg
Pulse rate : 74bpm, normal volume, regular
Respiratory rate : 15cpm
Temp : Afebrile to touch
No pallor , icterus, cyanosis, clubbing, lymphadenopathy, edema.
No neurocutaneous markers
SYSTEMIC EXAMINATION:-
CNS EXAMINATION:-
Higher mental functions intact- conscious, oriented to time place and person
Speech - no aphasia , dysphonia, dysarthria
Fluency, repetitions, naming - intact
No delusions and hallucinations
No signs of meningeal irritation
GCS scale - 15/15
Gait - walks with support
Cranial nerves:-
1 no alternation in smell
2 visual activity normal
3,4,6 - eye movements in all directions
5 - normal sensations on face , mastication- normal, corneal reflex - normal
7 - deviation of mouth towards left side
8 - no hearing impairment, vertigo and nystagmus absent
9,10 - no difficulty in swallowing , no deviation of uvula, gag reflex +
11 - normal neck movements
12 - tongue movements normal, no deviation of tongue
Pupils - normal in size , reactive to light
Motor system
Bulk
TONE :
Rt Lt
UL Increased N
LL Increased N
POWER:-
Rt Lt
UL 4/5 5/5
LL 4/5 5/5
REFLEXES:
Rt Lt
Biceps +++ ++
triceps +++ ++
supinator ++ ++
knee +++ ++
ankle +++ ++
plantar extension flexion
Gait - not able to walk properly , need support while walking
Involuntary movements - absent
Fasciculation - absent
SENSORY SYSTEM-
Pain, temperature, crude touch, pressure sensations normal
Fine touch, vibration, proprioception normal
No abnormal sensory symptoms
Cerebellum -
Finger nose test normal, no dysdiadochokinesia, no intentional tremor, Romberg test could not be done
Spine and cranium - no deformities
CVS EXAMINATION :-
JVP: Normal
INSPECTION:
Chest wall symmetrical
Trachea central
PALPATION:
Apical impulse felt
Thrills absent
PERCUSSION:
No abnormal findings
AUSCULTATION:
S1, S2 heard
No murmurs
ABDOMINAL EXAMINATION :-
INSPECTION:
Flat shaped, free flanks , umbilicus central and normal in shape, hernial orifices normal
PALPATION:
Abdomen is soft and non tender, no hepatomegaly, no splenomegaly
Kidneys not enlarged, no renal angle tenderness
PERCUSSION:
Fluid Thrill/Shifting dullness/Puddle’s sign absent
AUSCULTATION:
Bowel sounds – normal
No bruits
RESPIRATORY EXAMINATION :-
Chest bilaterally symmetrical, all quadrants
moves equally with respiration.
Trachea central, chest expansion normal.
Resonant on percussion
Bilateral equal air entry, no added sounds heard.
Normal Vesicular Breath sounds heard.
Norm vocal resonance.
Vocal Resonance - normal
PROVISIONAL DIAGNOSIS:-
Acute Cerebrovascular accident ,mostly infarct in left internal capsule involving left MCA territory
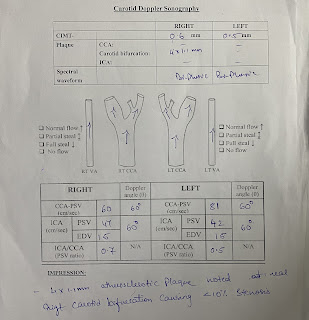
INVESTIGATIONS:
Anti HCV antibodies rapid - non reactive
HIV 1/2 rapid test - non reactive
Blood sugar random - 109 mg/dl
FBS - 114 mg/dl
Haemoglobin- 13.4 gm/dl
WBC-7,800 cells/cu mm
Neutrophils- 70%
Lymphocytes- 21%
Eosinophils- 01%
Monocytes- 8%
Basophils- 0
PCV- 40 vol%
MCV- 89.9 fl
MCH- 30.1 pg
MCHC- 33.5%
RBC count- 4.45 millions/cumm
Platelet counts- 3.01 lakhs/ cu mm
SMEAR:
RBC - normocytic normochromic
WBC - with in normal limits
Platelets - Adequate
Haemoparasites - no
CUE:
Colour - pale yellow
Appearance- clear
Reaction - acidic
Sp.gravity - 1.010
Albumin - trace
Sugar - nil
Bile salts - nil
Bile pigments - nil
Pus cells - 3-4 /HPF
Epithelial cells - 2-3/HPF
RBC s - nil
Crystals - nil
Casts - nil
Amorphous deposits - absent
LFTs:
Total bilirubin - 1.71 mg/dl
Direct bilirubin- 0.48 mg/dl
AST - 15 IU/L
ALT - 14 IU/L
Alkaline phosphatase - 149 IU/L
Total proteins - 6.3 g/dl
Albumin - 3.6 g/dl
A/G ratio - 1.36
Blood urea - 19 mg/dl
Serum creatinine - 1.1 mg/dl
Electrolytes
Sodium - 141 mEq/L
Potassium - 3.7 mEq/L
Chloride - 104 mEq/L
Calcium ionised - 1.02 mmol/L
USG:-
TREATMENT:-
1. INJ. OPTINEURON 1 AMP IN 100ML NS IV/OD
2. TAB. ECOSPRIN AV 75/10 PO/HS
3. TAB. CLOPITAB 75 MG PO/OD
4. PHYSIOTHERAPY OF RIGHT UPPER AND LOWER LIMB
5. SYRUP. CREMAFFIN PLUS 15ML PO/HS






Comments
Post a Comment