1801006118 - SHORT CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
A 38yr old male resident of West Bengal , civil engineer by occupation came to the OPD with chief complaints of abdominal pain since 5 years
HOPI :-
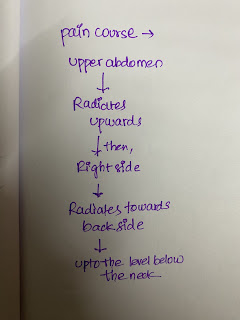
Patient was apparently asymptomatic 10days back then developed pain abdomen which is sudden in onset , gradual in progression , dragging type radiating to back which aggravates on intake of food, alcohol and relieved on medication.
H/o episodes of vomiting followed by pain in abdomen at least once in 2 days which is non bilious and water as content associated with weakness and giddiness
he had multiple episodes of vomiting after lunch, initially vomiting containing food particles (yellowish) later watery associated with weakness and giddiness and not relieved on
He also complains of severe weight loss.
H/o accident 1 year ago, injured at elbow and knee, dental injury
Patient also complains of constipation and per rectal bleeding since childhood.
Daily routine: He wakes up at 6am in the morning , have breakfast ,go to the office ,completes his work and returns by 5pm and plays badminton or football and then comes to home ,have dinner at 8pm and goes to bed by 10pm
Past history:-
Known case of haemorrhoids since 12 years of age
History of jaundice when he was 12 years old which later subsided
History of trauma to the nose while playing football during childhood (15 years) and developed Deviated nasal septum towards left side.
H/o Appendicectomy when he was 17 years old
H/o leprosy 12 years ago
N/K/C/O DM, Hypertension,TB, Asthma, epilepsy
H/o psychiatric problem- depression, insomnia which not subsided on medication
Family History:-
Not Significant
Personal History:-
Diet - Mixed
Appetite - Normal.
Sleep - Inadequate
B&B - Bowel - constipation since 12 years old
Bladder movements normal
Addictions - Alcohol - 180mL to 375mL everyday from 10 years. From last 6months he decreased consuming alcohol
Smoking - Initially 2 packs per day back when he was in college later 1 pack per day
Allergic History :-
Not allergic to any food or drug
Treatment History:-
Anti anxiety drugs
Medications to induce sleep- atiavin 2mg
Ayurvedic medicine( Jandu?) for constipation
Tramadol for pain
GENERAL EXAMINATION -
Patient was conscious, coherent, cooperative and well oriented to time, place and person
Moderately built and nourished
Pallor , icterus , cyanosis , clubbing , lymphadenopathy , edema - ABSENT
Temperature 94F
PR :- 80bpm
RR :- 16cpm
BP :- 110/70 mmHg
SpO2 :- 98%
SYSTEMIC EXAMINATION:-
CVS - S1 , S2 heard, No murmurs
RS - B/L airway entry + , Normal vesicular breath sounds - heard
CNS - No focal and neurological deficits
P/A
Inspection: Not distended , umblicus inverted , No discharging sinus seen, Scar in the RIF ( Appendicectomy), no dilated veins.
Palpitation : No local rise in temperature, Mild tenderness in epigastric region, No organomegaly
Percussion: tympanic
Auscultation: Bowel sounds audible
BURSA can be felt on palpitation at elbow and hip areas
PROVISIONAL DIAGNOSIS : acute pancreatitis
INVESTIGATIONS:-
CBP
HB 11.2 gm/dl
total count 4700 cells/Cumm
Neutrophil 64%
Lymphocytes. 22%
Monocytes. 2%
Basophils 1%
Smear normocytic normochromic
Liver functional test
Total Bilirubin 1.53mg/dl
AST 42 IU/L
ALT 72 IU/L
ALP 1243 IU/L
Total proteins 5.3gm/dl
Albumin 2.98GM/DL
Serum lipase 72IU/L
Serum amylase 176 IU/L
CT ABDOMEN:-
USG Right elbow-
Features of mild Right Olecranon bursitis
TREATMENT:
1.T.ULTRACET
2.BP MONITORING
3.VITALS MONITORING 6TH HRLY

















Comments
Post a Comment